If you have an irregular heartbeat (arrhythmia), your doctor might ask you to have an electrophysiology study. This procedure will allow your doctor to assess any issues you may have with the electrical activity in your heart, and identify how best to address it.
This procedure is sometimes referred to as an EP study of the heart, or an EPS. Find out more about why you might need to have an electrophysiology study and what to expect when having this procedure.
Key points
- An electrophysiology study assesses the electrical activity of the heart.
- An EPS enables doctors to diagnose abnormal heartbeats or arrhythmia.
- The test will enable your doctor to assess how best to treat your arrhythmia, either with medication, surgery, radiofrequency catheter ablation, an implantable cardioverter defibrillator, or a pacemaker.
What is an electrophysiology study?
An electrophysiology study will assess the electrical activity of your heart. The study analyses any abnormal heart rhythms and evaluates the effect of drug therapy. The electrical system of the heart is stimulated with electrode catheters, which are insulated wires with an electrode at the tip.
“During an electrophysiology study, your heart’s electrical system is recorded, and the information is then analysed,” says Dr Sean Gomes, Procedural Cardiologist at Eastern Heart Clinic.
“This information helps your cardiologist diagnose an abnormality in your heat and determine the most appropriate treatment.”
Why do I need an electrophysiology study?
Your doctor might suggest an EPS if you have problems with your heart rhythm, such as irregular heartbeats, or a heart that beats too quickly or slowly. You might also need one if you have a heart condition that has the potential to cause a cardiac arrest, or you have fainting episodes where you lose consciousness.
Your heart pumps blood to the lungs and body thanks to electrical signals that come from specific areas of the heart. The heart’s ‘pacemaker’ is the sinoatrial node, which is made up of cells that stimulate the left and right atrium (the upper chambers) to contract and push blood into the ventricles (the lower chambers). The electrical impulses then travel to the ventricles and make them contract, pumping blood to the lungs and body. In a healthy heart, those electrical signals travel through the heart in a regular rhythm.
“When there’s a problem with the heart’s ability to transmit electrical impulses, or these impulses are blocked, this may result in the heart beating too slowly, too quickly, or with irregular beats,” Dr Gomes says.
“Some common effects of these heart rhythm disturbances are dizziness, fainting spells or palpitations.”
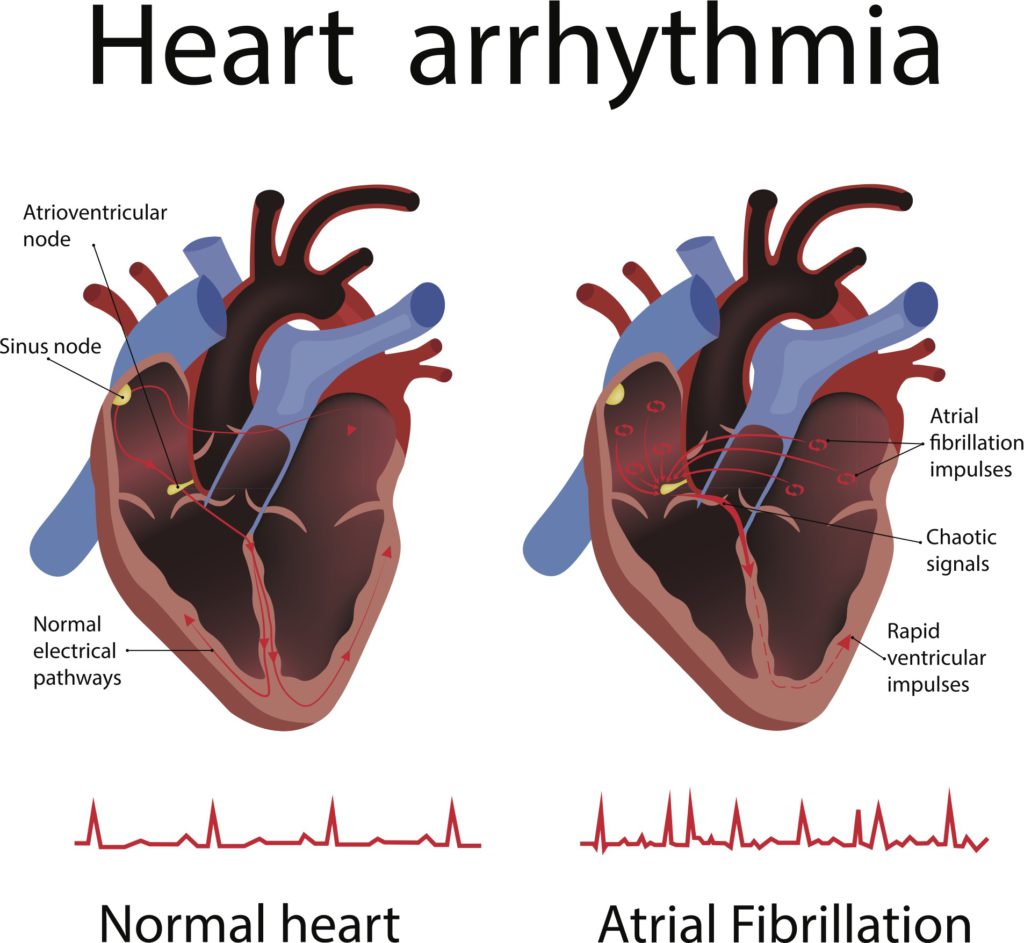
The heart’s ‘pacemaker’ is the sinoatrial (or sinus) node, which creates electrical signals that keep the heart pumping. If there’s a problem with your heart’s ability to transmit electrical impulses, or if these impulses are blocked, it can lead to arrhythmias.
What are the risks?
Like with all procedures, there are some risks associated with having an EPS. These include:
- Abnormal heart rhythms during the test, which can make you feel dizzy. If necessary, your doctor will give your heart an electric shock to restore a regular heartbeat.
- Bleeding, bruising or infection at the site where the catheter is inserted in the groin or arm.
- Blood clots in the legs or lungs. You may be given medication to prevent blood clots.
- Bleeding around the heart, or damage to the blood vessels or heart valves.
- Heart attack or stroke.
Everything will be done to minimise these risks during the procedure. Talk to your doctor if you’re concerned.
What happens:
Before
You’ll need to stop eating food six hours before the test, and stop drinking any clear fluids two hours before the procedure. If you’re taking any medication such as blood thinners or diabetes medication, your doctor will let you know whether to stop or change your dosage before the test.
During
Your doctor will inject local anaesthetic into the skin in the groin area (and occasionally in the arm). Once the skin has been anaesthetised, a small tube is placed in the vein. Guided by an x-ray image, electrode catheters will be inserted – you should only feel minimal discomfort – and positioned at specific locations in the heart.
Your doctor will send electric signals through the catheters to speed up or slow down your heartbeat. Electric signals produced by your heart will be recorded, indicating whether there is an arrhythmia and where it’s coming from.

Our expert team will look after you at every stage of the procedure.
After
After the study is finished, the catheters will be removed and the doctor will apply pressure and a dressing to the wound. You’ll need to stay in recovery and rest afterwards for about four hours.
The study will take about one hour, but you’ll need to be at the clinic for six to eight hours from the time of admission to time of discharge.
You might be able to go home the same day, but you’ll need someone to drive you home or accompany you if you are travelling by taxi or uber. You might feel sore for a few days where the catheters were inserted.
How long does it take to recover afterwards?
You should be able to start doing your normal activities a few days after the procedure.
“Your doctor will discuss the results of your test and let you know the best treatment for you,” Dr Gomes says.
About Eastern Heart Clinic
Eastern Heart Clinic is an interventional cardiology hospital co-located at the Prince of Wales Hospital at Randwick in Sydney’s eastern suburbs.
One of the largest interventional cardiology hospitals in New South Wales, Eastern Heart Clinic provides diagnostic and interventional cardiology services to public and private patients in metropolitan Sydney and New South Wales.
Learn more about our clinic, cardiology procedures, and what to expect if you’ll be visiting us for a procedure.
Read more:


Recent Comments